Participating in a rehabilitation program is a very important part of living with Parkinson’s disease. The goal of rehabilitation is not to reverse the effects of Parkinson’s—as this is not always possible—but rather to slow down the degenerating effects of the disease. Rehabilitation helps target symptoms and maximizes the ability to function efficiently despite symptoms. Your physiotherapist typically aims to keep an individual as independent as possible for as long as possible. There may also be specific lifestyle goals that a physiotherapist can help with.

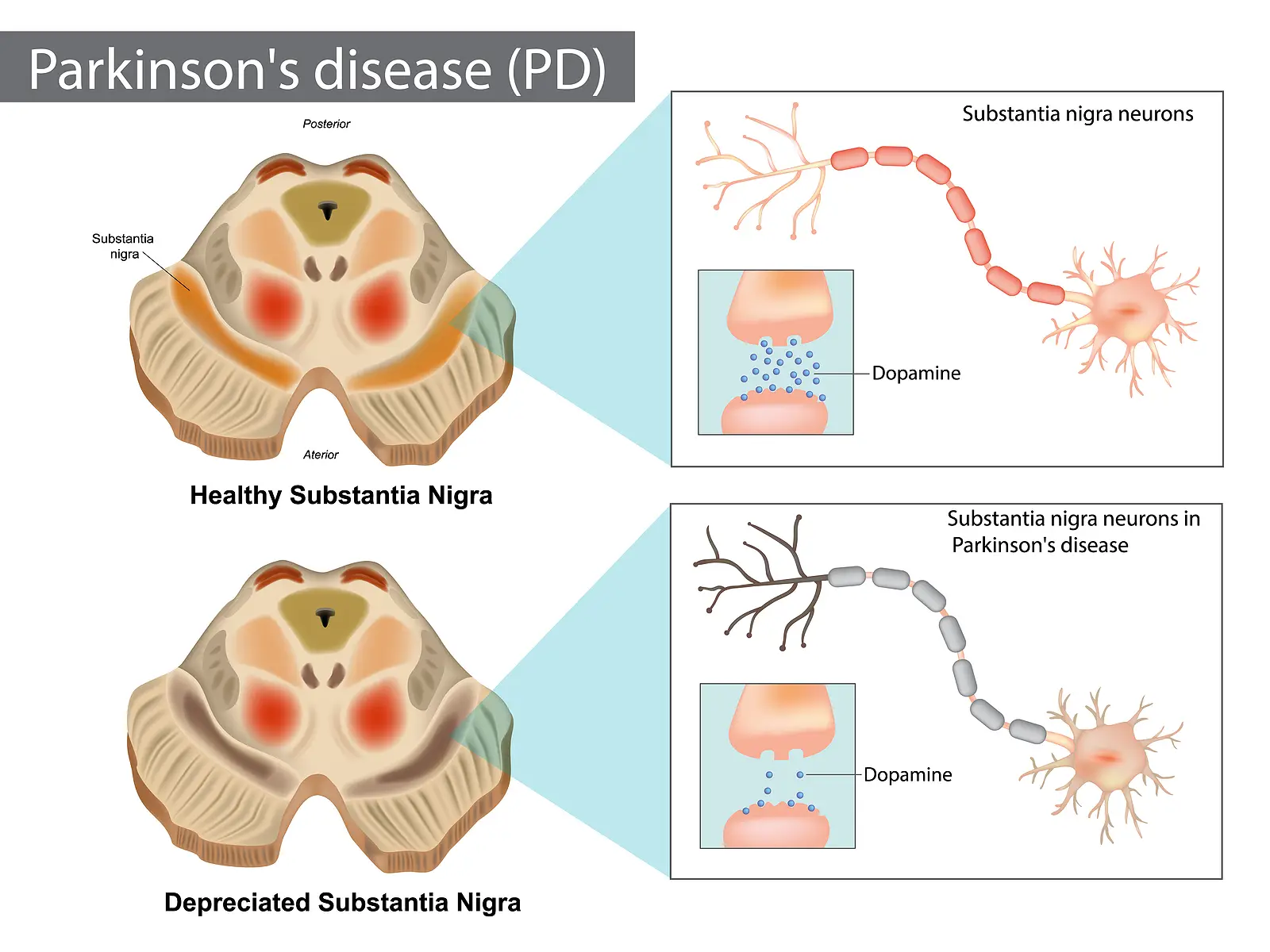
Regular exercise is important for everyone, but research shows that exercise is particularly effective for people living with Parkinson’s, as it can affect how well dopamine is used in the brain.
Every Parkinson’s disease journey is different, so a physiotherapist will focus on developing an individualized exercise program that minimizes specific symptoms (e.g., tremors, stability issues, writing difficulties). Exercise for people with Parkinson’s may also include a combination of exercises for strength, balance, endurance, flexibility, and coordination. Several exercise techniques may be used by your physiotherapist to establish a therapeutic regimen.
Therapeutic Exercises
Cardiovascular (aerobic) exercise:
Several studies have shown the benefits of high-intensity exercise, as this type of activity slows the general aging of the brain in healthy adults. High-intensity exercise is defined as exercise that raises the heart rate and promotes deeper breathing. In people with Parkinson’s, high-intensity aerobic exercise also helps slow down motor skill degeneration, protects against depression, and improves quality of life.
Your physiotherapist can recommend what type of high-intensity exercise might be the most beneficial, the degree to which it should be performed, and how often to exercise. The consensus is that the more cardiovascular exercise an individual performs, the better! This means that even small amounts of exercise count!
As a guide, one study showed that about 2.5 hours of physical activity each week slowed the decline in quality of life in people living with Parkinson’s disease. It is helpful to choose a form of exercise that is enjoyable, and consistency is the key. Enhanced benefits have been observed with exercise programs that are six months or longer in comparison to programs that only last for a few weeks or months.
Strength training: Using weights can also be beneficial in improving strength, particularly lower body strength—an important aspect of health that has a direct effect on the ability to maintain balance. In addition, both upper and lower body strength training has been shown to help decrease slowness of movement (bradykinesia), which may be a symptom for some people with Parkinson’s. In addition, strength training can improve the ability to move more easily and perform regular daily activities.
Balance, posture, and fall prevention: The loss of healthy dopamine levels affects the ability to initiate or make continuous movements. Sometimes it is difficult for people with Parkinson’s disease to start a movement (akinesia), or movements are slow (bradykinesia). Furthermore, movements that are normally automatic are also affected, such as blinking, swallowing, walking while talking, or arm swinging with walking. Individuals with Parkinson’s may also have to be reminded to continue these types of movements.
A change in the ability to initiate movements or having slower and fewer automatic movements can directly affect posture and balance. This can in turn increase the risk of falling. It has been well proven that balance can improve with training! For this reason, a physiotherapist will work on posture and balance exercises. Your physiotherapist will also discuss strategies that make regular activities less risky for falls and the home environment safer.
Movement strategy training: Different types of movement training can assist with maintaining regular motion and regulating automatic movements. Therefore, your physiotherapist may work on reciprocal training, which aims at reintegrating normal reciprocal movements such as arm swinging and trunk rotation with walking. It has also been shown that training with oversized movements, such as exaggerated arm or leg swings or taking extra-large steps when practicing, can help maintain smaller, similar movements that are normal with everyday activities. Your physiotherapist may also actively train an individual with Parkinson’s through activities that involve performing two tasks at once (dual-task training), such as walking and carrying a cup of water, walking and talking, or walking while doing mental tasks. Using mental imagery to imagine the appropriate movement may also be used to assist the rehabilitation process.
Additional Activities: Additional activities such as dancing, non-contact boxing, tai chi, qi-gong, biking, and yoga have all been shown to help target symptoms of Parkinson’s disease. As a result, a physiotherapist may incorporate these types of activities into the exercise routine. In addition, your physiotherapist may encourage participation in group exercise or a support group. It is well proven that group activities can positively benefit overall well-being. This is also true for people with Parkinson’s.
Interdisciplinary Team Therapy
Physiotherapists may recommend working with other healthcare professionals to better address specific rehabilitation needs. For instance, they may suggest speaking with an occupational therapist (OT) who can focus on fine motor tasks required for daily living activities such as getting dressed, bathing or showering, writing, cooking, and any other activities an individual may be struggling with. They can also assist with advice regarding home modifications that can help reduce fall risks or provide support to foster independence.
Your physiotherapist may also suggest a consultation with a speech-language pathologist (SLP) to address symptoms such as poor voice projection, speech difficulties, swallowing concerns, diminishing facial expressions, or communication problems.
Research regarding additional therapeutic exercises, training techniques, and rehabilitation methods that may benefit individuals with Parkinson’s disease is ongoing.
 This guide will help you understand:
This guide will help you understand:
 To date, there is no single test that can accurately identify the presence of Parkinson’s disease. Instead, the diagnostic procedure involves assessing medical history, presenting symptoms, neurological tests, and a physical examination that a healthcare professional conducts.
Although Parkinson’s disease is often diagnosed when the classic motor (movement) signs or symptoms are present such as tremors, muscle rigidity, balance issues, festinating gait, or difficulty moving, current research points to the identification of non-motor signs. More specifically, signs such as the loss of smell, dizziness, constipation, sleep disturbances, and depression often become evident ahead of the motor-related signs and can potentially be used for earlier diagnosis of the disease in the future.
If a healthcare professional suspects Parkinson’s disease, the next step is a referral to a doctor who specializes in neurological disorders, such as a neurologist.
To date, there is no single test that can accurately identify the presence of Parkinson’s disease. Instead, the diagnostic procedure involves assessing medical history, presenting symptoms, neurological tests, and a physical examination that a healthcare professional conducts.
Although Parkinson’s disease is often diagnosed when the classic motor (movement) signs or symptoms are present such as tremors, muscle rigidity, balance issues, festinating gait, or difficulty moving, current research points to the identification of non-motor signs. More specifically, signs such as the loss of smell, dizziness, constipation, sleep disturbances, and depression often become evident ahead of the motor-related signs and can potentially be used for earlier diagnosis of the disease in the future.
If a healthcare professional suspects Parkinson’s disease, the next step is a referral to a doctor who specializes in neurological disorders, such as a neurologist.
 Regular exercise is important for everyone, but research shows that exercise is particularly effective for people living with Parkinson’s, as it can affect how well dopamine is used in the brain.
Every Parkinson’s disease journey is different, so a physiotherapist will focus on developing an individualized exercise program that minimizes specific symptoms (e.g., tremors, stability issues, writing difficulties). Exercise for people with Parkinson’s may also include a combination of exercises for strength, balance, endurance, flexibility, and coordination. Several exercise techniques may be used by your physiotherapist to establish a therapeutic regimen.
Therapeutic Exercises
Cardiovascular (aerobic) exercise:
Several studies have shown the benefits of high-intensity exercise, as this type of activity slows the general aging of the brain in healthy adults. High-intensity exercise is defined as exercise that raises the heart rate and promotes deeper breathing. In people with Parkinson’s, high-intensity aerobic exercise also helps slow down motor skill degeneration, protects against depression, and improves quality of life.
Your physiotherapist can recommend what type of high-intensity exercise might be the most beneficial, the degree to which it should be performed, and how often to exercise. The consensus is that the more cardiovascular exercise an individual performs, the better! This means that even small amounts of exercise count!
As a guide, one study showed that about 2.5 hours of physical activity each week slowed the decline in quality of life in people living with Parkinson’s disease. It is helpful to choose a form of exercise that is enjoyable, and consistency is the key. Enhanced benefits have been observed with exercise programs that are six months or longer in comparison to programs that only last for a few weeks or months.
Strength training: Using weights can also be beneficial in improving strength, particularly lower body strength—an important aspect of health that has a direct effect on the ability to maintain balance. In addition, both upper and lower body strength training has been shown to help decrease slowness of movement (bradykinesia), which may be a symptom for some people with Parkinson’s. In addition, strength training can improve the ability to move more easily and perform regular daily activities.
Balance, posture, and fall prevention: The loss of healthy dopamine levels affects the ability to initiate or make continuous movements. Sometimes it is difficult for people with Parkinson’s disease to start a movement (akinesia), or movements are slow (bradykinesia). Furthermore, movements that are normally automatic are also affected, such as blinking, swallowing, walking while talking, or arm swinging with walking. Individuals with Parkinson’s may also have to be reminded to continue these types of movements.
A change in the ability to initiate movements or having slower and fewer automatic movements can directly affect posture and balance. This can in turn increase the risk of falling. It has been well proven that balance can improve with training! For this reason, a physiotherapist will work on posture and balance exercises. Your physiotherapist will also discuss strategies that make regular activities less risky for falls and the home environment safer.
Movement strategy training: Different types of movement training can assist with maintaining regular motion and regulating automatic movements. Therefore, your physiotherapist may work on reciprocal training, which aims at reintegrating normal reciprocal movements such as arm swinging and trunk rotation with walking. It has also been shown that training with oversized movements, such as exaggerated arm or leg swings or taking extra-large steps when practicing, can help maintain smaller, similar movements that are normal with everyday activities. Your physiotherapist may also actively train an individual with Parkinson’s through activities that involve performing two tasks at once (dual-task training), such as walking and carrying a cup of water, walking and talking, or walking while doing mental tasks. Using mental imagery to imagine the appropriate movement may also be used to assist the rehabilitation process.
Additional Activities: Additional activities such as dancing, non-contact boxing, tai chi, qi-gong, biking, and yoga have all been shown to help target symptoms of Parkinson’s disease. As a result, a physiotherapist may incorporate these types of activities into the exercise routine. In addition, your physiotherapist may encourage participation in group exercise or a support group. It is well proven that group activities can positively benefit overall well-being. This is also true for people with Parkinson’s.
Regular exercise is important for everyone, but research shows that exercise is particularly effective for people living with Parkinson’s, as it can affect how well dopamine is used in the brain.
Every Parkinson’s disease journey is different, so a physiotherapist will focus on developing an individualized exercise program that minimizes specific symptoms (e.g., tremors, stability issues, writing difficulties). Exercise for people with Parkinson’s may also include a combination of exercises for strength, balance, endurance, flexibility, and coordination. Several exercise techniques may be used by your physiotherapist to establish a therapeutic regimen.
Therapeutic Exercises
Cardiovascular (aerobic) exercise:
Several studies have shown the benefits of high-intensity exercise, as this type of activity slows the general aging of the brain in healthy adults. High-intensity exercise is defined as exercise that raises the heart rate and promotes deeper breathing. In people with Parkinson’s, high-intensity aerobic exercise also helps slow down motor skill degeneration, protects against depression, and improves quality of life.
Your physiotherapist can recommend what type of high-intensity exercise might be the most beneficial, the degree to which it should be performed, and how often to exercise. The consensus is that the more cardiovascular exercise an individual performs, the better! This means that even small amounts of exercise count!
As a guide, one study showed that about 2.5 hours of physical activity each week slowed the decline in quality of life in people living with Parkinson’s disease. It is helpful to choose a form of exercise that is enjoyable, and consistency is the key. Enhanced benefits have been observed with exercise programs that are six months or longer in comparison to programs that only last for a few weeks or months.
Strength training: Using weights can also be beneficial in improving strength, particularly lower body strength—an important aspect of health that has a direct effect on the ability to maintain balance. In addition, both upper and lower body strength training has been shown to help decrease slowness of movement (bradykinesia), which may be a symptom for some people with Parkinson’s. In addition, strength training can improve the ability to move more easily and perform regular daily activities.
Balance, posture, and fall prevention: The loss of healthy dopamine levels affects the ability to initiate or make continuous movements. Sometimes it is difficult for people with Parkinson’s disease to start a movement (akinesia), or movements are slow (bradykinesia). Furthermore, movements that are normally automatic are also affected, such as blinking, swallowing, walking while talking, or arm swinging with walking. Individuals with Parkinson’s may also have to be reminded to continue these types of movements.
A change in the ability to initiate movements or having slower and fewer automatic movements can directly affect posture and balance. This can in turn increase the risk of falling. It has been well proven that balance can improve with training! For this reason, a physiotherapist will work on posture and balance exercises. Your physiotherapist will also discuss strategies that make regular activities less risky for falls and the home environment safer.
Movement strategy training: Different types of movement training can assist with maintaining regular motion and regulating automatic movements. Therefore, your physiotherapist may work on reciprocal training, which aims at reintegrating normal reciprocal movements such as arm swinging and trunk rotation with walking. It has also been shown that training with oversized movements, such as exaggerated arm or leg swings or taking extra-large steps when practicing, can help maintain smaller, similar movements that are normal with everyday activities. Your physiotherapist may also actively train an individual with Parkinson’s through activities that involve performing two tasks at once (dual-task training), such as walking and carrying a cup of water, walking and talking, or walking while doing mental tasks. Using mental imagery to imagine the appropriate movement may also be used to assist the rehabilitation process.
Additional Activities: Additional activities such as dancing, non-contact boxing, tai chi, qi-gong, biking, and yoga have all been shown to help target symptoms of Parkinson’s disease. As a result, a physiotherapist may incorporate these types of activities into the exercise routine. In addition, your physiotherapist may encourage participation in group exercise or a support group. It is well proven that group activities can positively benefit overall well-being. This is also true for people with Parkinson’s.
